Thursday 13th February, and another appointment. Once again, at the Queen Alexandra Hospital. I’ll soon have my own allocated parking space if my visits carry on at this rate.
This time my appointment is with an anaesthetist in the Outpatients department.
My appointment was at 10:00, and right on the button, I was whisked away for some observations. I had my blood pressure, weight, and height measured, again. I was also given an ECG. And then it was back to the waiting room where I had time to make friends, playing peek-a-boo with a toddler.
After a short while my name was called by the anaesthetist wearing an amazing pair of electric blue shoes.
After the usual pleasantries she revealed that we had met before. Ten years ago, when I went in for the brachytherapy treatment for my prostate. She was the anaesthetist who drew the short straw for my procedure. As a patient I was not very cooperative, not on purpose. With me sat on the table in theatre she attempted to give me an epidural. Three times!! My body just refused to play ball, would not give up my spinal fluid so no further attempts were made.
Once the procedure was underway it was time for me to misbehave again. I unconciously decided to vomit. She unfortunately had to deal with that, and call in Dynarod to suck out my tubes.
I apologised to her as in my head I was to blame, having had rather a lot of cheese as my last meal the night before the procedure. Nobody told me that they tilted you head down to insert the nuclear seeds. She showed me the copious notes taken following that little episode but she was quite magnanimous. Noting my, as yet undiagnosed, type 2 diabetes which apparently can have the effect of slowing down your stomach process, causing “pooling” which in turn can cause regurgitation.
After reminiscing about old times we got down to the business in hand. We had the inevitable chat about my health in general and specifically focussing on weight, fitness and diet.
I was given a thorough but gentle arse kicking. Likening preparing for the operation to an athlete preparing for the olympics. Apparently the procedure will last about four hours and, although I will be unconcious laid out on the table, for my body it will be akin to running against Usain Bolt. So, as she put it, I need to be in the best possible shape to deal with the procedure but also the fitter I am the faster I will recover.
Exercise and weight loss are the order of the day, supplemented by plenty of practice with my spirometer. She wants me to up my daily walking. That shouldn’t be hard since it is negligible at the moment.
We also talked about diet with regard to my diabetes which can have a negative impact on my post op recovery. And right there is where I get into trouble.
In general the medics extol the benefits of a balanced diet, with plenty of fruit, vegetables, nuts, seeds and so forth. Quite often promoted as the mediterranean diet. Below is a typical chart promoting a balance diet. All stuff that I like.
Due to the location of my tumour which is partially blocking my bowel I have been advised to stay on a low residue diet which conflicts with the idea of a balanced diet. Which in turn also conflicts with a diabetic friendly diet.
What that means is that the only food that I can eat from the green zone is carrots which have been peeled and cooked until they are soft. I can have cucumber but I have to peel it and scoop out the seeds. From the yellow zone I cannot eat any of the wholegrain items. I can have potatoes cooked without their skins and not shown I can have white bread, rice and pasta.
Hang on a bit, actually, for my diabetes I should not be eating any quantity of carbohydrates as this gets turned into sugar, bad for diabetics. So between the diabetes and my tumour everything in the yellow zone is pretty much a no-no.
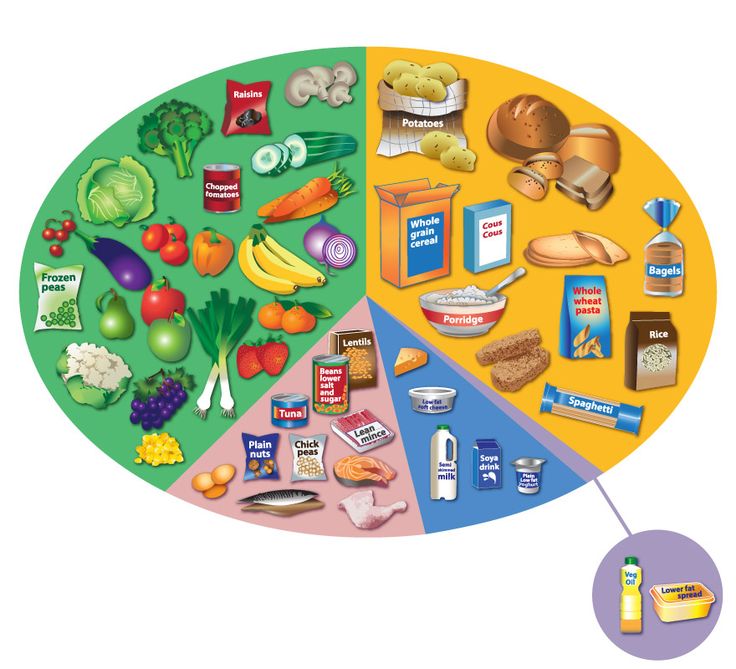
Things do get a little better when we look at that strange pink zone. I can eat the tinned tuna, chicken, fish, eggs, and mince. Although my tumour says no to fish skin and bones like you might get with sardines and pilchards. Meat is fine but no gristly bits, no bacon rind etc.
And on to the blue zone where I am allowed small amounts of cheese and milk.
And so, I am resigned to eating a mainly protein diet, not quite leaping into the full carnivor diet. Supplemented by squidgy overcooked root vegetables.
As if meal preparation wasn’t already difficult enough.
Ah well, as the anaesthetist says, it is only for a few weeks.
Sad to say, I still don’t have a date for my op.
