Informational Links:
http://www.huffingtonpost.co.uk/2013/01/22/prostate-cancer-rates-treble_n_2527232.html#slide=1761849
Part 1
Here I am in my 60th year. I have made it through most of my adult life without suffering anything worse than the common cold and the occasional bout of flu. A couple of years back I was diagnosed with hypertension and have been taking tablets ever since to keep things under control. All has been well until earlier this year when I was asked to provide a blood sample as part of the regular monitoring. This time my GP said he noted that I hadn’t been checked for prostate cancer so he added it to the list of things for the lab to check out. He told me to call in a couple of weeks to find out the results.
Me being me, I forgot all about it and did nothing.
Some time later I decided to go and see the doctor about a couple of moles on my shoulder. During the exam I mentioned the blood test and asked about the prostate element. After he pulled up my notes and following some chin rubbing he said “Your PSA is up a bit, perhaps we should book you in for an examination” So I was left to go and make an appointment. While I am at the reception desk he calls me back in to the examination room. “Since you are here we might as well do it now” he says. A few minutes later he’s got a rubber glove on and I’m laid down on the couch, facing the wall with my knees tucked up under my chin.
After a strange and unusual experience he informs me that his exam was inconclusive, that he really isn’t an expert and feels it would be better if I was examined by someone with more experience. Personally I would rather that he had chosen someone else to gain experience with.
A week or two later I am up at The QA (Queen Alexandra hospital, Portsmouth) and I’m laid down on a couch, facing a different wall, with my knees tucked up under my chin. This time it is the lovely Vanessa with the rubber glove. This time I’m told that because I am tall, my prostate is quite high up and she thinks that we should have another blood test to compare with my earlier one and based on that, a decision would be made as to the need for a biopsy.
An appointment date is set and I am left to arrange a visit to the vampires at my GPs practice. I manage to fit in a fortnights holiday in between times, get the blood drawn and await the results.
On Thursday, July 26th, I have a short but vibrant telephone call with Vanessa who informs me that my PSA is once again elevated, that it is probably nothing, but why don’t we have a biopsy just to be sure.
An appointment is made for Tuesday, July 31st. All too soon I am sitting in the waiting room and my name is called. They hadn’t warned me, but en-route to the torture chamber, they ask me to provide a urine sample. If I had known I would have made sure that I had plenty to drink. Needless to say I could not perform. Not a drop. “Stage Fright” says Vanessa.
Once again I find myself with my trollies down round my ankles, laid down on a couch, facing yet another wall, with my knees tucked up under my chin and my bum hanging over the edge. Now that’s an image to scare the kiddies don’t you think.
So the procedure gets underway, the ultrasound wand is put where the sun doesn’t shine, anaesthetic is applied and the numerous biopsy samples are taken with the device clacking away with the sound of an industrial stapler. Job done, my bum is wiped and a man sized pantyliner applied and I am packed off home, advised not to do anything strenuous. As if.
Thursday, August 30th, and I am once again at the QA. This time I am seeing Dr Dominic Hodgson. Where is the lovely Vanessa ? My name is called, introductions made and I am sitting waiting for Dr Hodgson to give me the “All Clear”.
So it’s all a bit surreal when he tells me that the biopsy has shown that I do in fact have Prostate Cancer.
Part 2
Some of you may have read my previous post on this subject. I realise that I left it as something of an open-ended, cliff edge item. I had intended to follow-up fairly quickly with the following but for some reason I found I couldn’t seem to find the time ??? Yet I managed to post on other matters. Go figure.
Since I am on the cusp of the next stage I felt I should bring this up to date, so here goes.
18 Months ago (or so) ….
….. after informing me that I did in fact have Prostate Cancer, Dr Hodgson proceeded to give me the details. The results of the biopsy and so forth. I think I am taking it all on board but in reality the enormity of my situation is quite overwhelming. Its only when he gets up and leaves the room in search of some leaflets that I really feel something. I’m not sure what it is but I have the sensation that something has just come down over me, like a sheet sliding over me. Not heavy but just there.
Dr Hodgson returns and we talk over things for a while longer. The net of this is as follows:
My biopsy has shown that I have Prostate Cancer, this is not good news, however you look at it.
I have a Gleason figure of 6 (3+3) 1% on the left side & 7 (3+4) 8% on the right side. This is relatively good news. Gleason figures in the 1 to 5 range are better. It is later explained to me that 3+4 is better than 4+3 even though they both add up to 7
I am 60 and, apparently, this is a good thing too as, with a following wind, I have maybe 30 -35 years ahead of me.
My options are :
- Surgery – Whip it out and chuck it away
- Radiotherapy – External High Energy X-rays
- Radiotherapy – Brachytherapy (Nuclear bullets)
- Active Surveillance – Regular 6 monthly blood tests to monitor the PSA levels and an annual biopsy unless something changes.
The last was not offered as an option and I had to ask if it was available because I had read about it on the web. Dr Hodgson said that it was an option but he hadn’t offered it as at my age it was more likely that I would eventually have to take one of the other options.
So, I pondered a while then opted for option 4.
My main reasons are a strong fear of people cutting in to my bod. Well that one aside I am also concerned about possible side effects of surgery. After all the Prostate Cancer, isn’t causing me any pain or other symptoms at this time. Whereas, surgery could introduce me to a few negative issues. i.e. infection and damage to surrounding body parts including the bladder. Both of the Radiotherapy options come with potential negative effects which include bladder control which I am not about to give up just yet.
Nope, on the whole, I preferred the idea of Active Surveillance. And that is what we have been doing for the last eighteen months or so. Every six months or so I have had a blood test to measure the PSA and after each test I have had an appointment with a consultant. Each test, other than the last, has shown a slight increase in the PSA. The last showed a 0.1 decrease which in my book is negligible. At the last consultant review we discussed that part of the Active Surveillance regime is a regular biopsy.
And here we are. I am about to go into hospital for a “Template Biopsy”. Instead of grabbing their samples via the back passage, using an ultrasound probe with local anaesthesia, they will knock me out with a general anaesthetic and take many samples using a “template” grid to give them a more accurate idea of what is going on with my prostate. These samples are taken through the skin between the back passage and my undercarriage.
Personally I am really pleased that this will be carried out under GA.
So there you have it. I am about to go into hospital to be shot blasted in the gusset region with 20, 30 or 40 needles.
I will update you on how I get on, if and when I am able to sit down again. And here is a pretty flower for those of you traumatised by the idea of a template biopsy.
Part 3
Template Biopsy !
Monday was one of the longest days of my life. I was scheduled for a “Template Biopsy” which for the un-initiated is described thus …..
The template biopsy is carried out using an ultrasound probe which is passed into your back passage and samples of the prostate gland are obtained through the area of the skin between your scrotum and back passage called the perineum. The procedure is similar to a trans rectal biopsy which you will usually have had.
Let me tell you, from the recipients perspective, it is nothing like the TRUS (Trans rectal biopsy).
To start with my TRUS was carried out fully conscious by a specialist nurse, the lovely Vanessa. The main difference though is that I was in and out of the hospital within an hour or so. But that was 18 months ago or more.
Mondays procedure was to be carried out under general anesthetic, for which I am truly grateful. But lets scroll back the clock a little.
Early Monday morning, Very early
I was awake, some time in the wee small hours. Either I am worrying about the procedure, or this is the residuals of jet-lag acquired on our return from Oz just over a week ago. Perhaps a combination of both. I checked the clock at 04:00 and thereafter approximately on the hour until I got up just after 07:00. I was not allowed to have anything to eat but was allowed clear liquids to drink and had a black tea around 08:00. The taxi was due to pick me up at 11:30 so I was pottering around in the house killing time. It’s amazing how often I found myself by the bread bin thinking “I’ll just have some toast” or over by the cupboard staring at a packet of peanuts. My last eats had been around 21:00 the previous evening. Going without food for that length of time is not natural for me.
Eventually the taxi turned up, although not at my house but three doors away. Luckily I saw him out there. It could have been worse, the dispatcher at the taxi office misheard my address as Sistine and, had I not corrected him, the taxi would probably have been well on his way to Rome and the Vatican. Still, having ascertained that he was there for me I boarded and we set off. Twice I had to correct his directions back to the main road before I was sure we were going to the hospital. Mentally I was crossing my fingers, hoping that the surgeon had a better sense of direction than my erstwhile pilot.
Tedium Begins
And so, at 11:50, I checked in at the QA Day Surgery Admissions Reception. And thus began the long wait. It’s a bit like being on a long haul flight, hours of tedium broken up by announcements from the flight crew. In this case there was no food or drink.
After thirty minutes or so I was taken along to a small room. Here I was visited by the anaesthetist who interrogated, sorry, checked my details and gave me a brief summary of what to expect. He also arranged for some initial meds.
Shortly thereafter, around 13:00, a nurse arrived with my lunch. A cup of water and four tabs, 2 x paracetamol / 1 antacid and 1 stop you feeling sicky pill.
While I was downing this feast another nurse arrived, interrogated me again and checked my blood pressure and heart rate. My heart rate was right down at about 55 which I queried but is apparently normal for “someone of our age”. She later demonstrated her own readings which were similar, so that was alright then.
I was then left alone to my own devices. I read for a while, played hangman on my phone, read some more, got up and walked around my room, looked out the window , read some more. Well you get the picture. I believe I even had a nap for a few minutes. The window looked down on the back dock but there was nothing happening down there.
Around 16:00 a yet another nurse informed me that I was Mr. Hodgsons last patient and that I would be seeing him soon. Well I saw his registrar who introduced himself but I have no idea what his name was. His accent, he was English I think, was as indecipherable as his signature on the forms that he got me to sign. He went through the now familiar interrogation, during which Mr. Hodgson popped in, shook my hand and disappeared again.
Oh The Indignity
Twenty minutes later I was invited to go and get changed, by yet another nurse, who led me down to a room full of changing cubicles. This is where all dignity ends.
I am not a small guy at just over six feet tall and way over twenty stones (280lb / 127kg). The nurse threw me a smock and left the room. Needless to say the smock, of the tie at the back variety, did not fit well and I struggled to secure it. Although there was no mirror available I could tell by the cool air that most of my back and all of my bum was pretty much fully exposed. The nurse popped her head in and asked how I was getting on. When I explained that the smock didn’t fit and I was having trouble tying it she assumed a sympathetic air and replied “I shouldn’t worry, the first thing they’ll do is undo it”. I then settled down to fight with the compression stockings which when battle was over were rolled up to just below my knees. Wonderful!!
So there I am with my pale blue smock reaching from just below my chin, down to about two inches above the knee. Struggling to meet my sage green stockings, some two inches below my knees. All with my bum exposed to the rear.
The epitomy of sartorial elegance ? Nope, not a pretty picture.
Not to worry, I thought, I have my dressing gown which should bridge the gap. No such luck. To make sure that I was all bright and shiny for the hospital, my wife had washed and tumble dried it. I hadn’t worn it until now and yes, you’ve guessed, it had shrunk. At least it still closed at the front but the length was a sadly lacking being just a tad longer than the hospital smock. At least my back & bum were covered and therefore a little warmer.
I gathered my stuff and found the nurse, who then gathered up another guy (John) and led us through the hospital. Imagine my feelings as we passed through the first doorway into a public waiting area. I’m dressed like a freak and as we entered the waiting area all heads turned to see who had arrived. I thought later that it must have looked like me and John got dressed in the dark and swapped dressing gowns. His gown reached from neck to ankles and wrapped around him properly while mine was way too small. So, we made it through the waiting area without the gales of laughter I was expecting. Next we traversed the hospital to a stairwell where we descended to the floor below and were left in a new waiting room with one other guy and a TV. Here we waited for what seemed like ages but must have been about thirty to forty minutes. John and the other guy got the call and then eventually so did I.
Kim, not sure if she was a nurse or a doctor, arrived to lead me to the Operating Theatre suite. Once again I had to traverse the hospital through the public corridors and climb to the upper floors via the stairwell. At this point a cold draught, not Guiness, reminded me about the negative aspects of my attire as I climbed the stairs. The stairs with the open railings to the centre, the railings that gave a not so glorious view of my nether regions to the several people descending these same flights of stairs. One glance up by any of them and they would be scarred for life.
Nearly There
On arrival I am sat in another waiting area, just for few minutes, but my apprehension levels are rising. This is not how I imagined the process would work. All this walking and waiting followed by more walking and waiting. And then an assistant anaesthetist comes and interrogates me one more time and I am on my way. One more surprise was that I had to walk into the theatre and get on the table myself. A green bag is held out for me to dump my shoes and dressing gown into. As I take off the gown a nurse rushes across the room to shut the doors to the outside, to prevent my blushes or those of any outsiders I’m not so sure. Then I am on the table.
And They’re Off
When I entered the theatre there was a group of folks gathered in the corner. Presumably they were in a pre-scrum huddle discussing my procedure. Or maybe they were just discussing Pompeys abysmal record. As I hop on the table I suddenly become the centre of a hive of activity as the anaesthetist and his assistant close in to prepare me. Cannula in the back of the hand, heart monitors etc. then the anaesthetist is telling me that I will feel a coldness in my hand as he injects the first of two concoctions. I felt nothing and then he informs me that I may feel a little dizzy. I’m staring at the ceiling and the light panels suddenly seem to displace and the next thing I know is a voice over my shoulder is speaking and inviting me to cough.
Job Done
I open my eyes and I am in a different room, apparently job done. This is like taking a shot with an SLR. You look through the lens, focus, shutter release, view goes blank as the mirror lifts, then the view is clear again when the mirror drops. All in the blink of an eye. I’m not feeling dopey or dizzy, just wide awake. Once the nurse is happy that I am OK I am wheeled through to a recovery area.
As I enter the new waiting area I pass John and the other guy from the pre-op waiting area. They are sitting up in their respective beds eating toast which they both wave at me.
After a short time and a cup of water I was invited to get dressed and was led outside to a seating area. The nurse asked if I had eaten anything or had a drink to which I responded “No”. I was offered coffee or tea and I was expecting toast but was in fact offered eggy or corned beef butties. John was already out there so I sat alongside and we compared notes as he had the same procedure. When my coffee and butties arrived he was rather envious since he was only offered toast and like me he loves corned beef. My wife was brought in and she eyed my butties hungrily too. She had been waiting outside since just after five and, as it was now gone seven, was very hungry.
The purpose of this little tea party is to ensure that you are OK, that you can keep down food and drink and most importantly that you can have a pee. If you can’t keep your food down or you don’t make water they won’t let you go home. Worst still an inability to pee can mean catheterisation and / or an overnight stay. Luckily I was able after a short while to produce a dribble. Oh but it burned. I’m guessing that I was catheterised during the procedure although nobody said.
Freedom
Anyway, based on my meager performance I was allowed to go and my daughter came and drove us home. Once home it was more tea and everyone seemed amazed, not the least of which me, at how alert I was. Also that I was in no pain. Well apart from when I had a pee which I was having to do with ever-increasing regularity.
Today, Wednesday Morning
Well the good news is that I have not had any pain. Two nights sleep, although still not sleeping all the way through so blaming the jet lag.
It is now nearly forty-one hours since the procedure. Any residual pain blocking by the anaesthetic must have worn off by now. The burning sensation has all but disappeared and I have a slight soreness in the perineum, like when you have a bruise, which only makes itself known when I sit on something hard.
Now I have to wait for approximately four weeks to hear the results. That brings us to Christmas week I think, so it is likely that my appointment will be after the holidays. We shall see.
Part 4
So, It’s been a while. Had a fairly intense conversation with a close friend last night. The intensity was about Steve Jobs and Apple, not my prostate, but that’s another story. Anyway during our conflab I was berated for not adding anything to my blog. In essence he was telling me off for leaving my story on another cliff edge.
As it happens I am approaching another significant milestone on this journey and by the time I finish this we’ll be at another cliff edge.
So here we go.
Consultations
Just before Christmas I had a meet with my consultant. Well one of them, seems I have three and they are not as entertaining as the Three Stooges, must be the subject matter. Anyway they take it in turns to see me.
I duly present myself at Urology Reception and after a short wait in the “General” waiting area we are ushered through to sit in a holding pattern outside the consultation rooms. I have been here a few times now and the wall opposite the seats isn’t getting any more interesting. Pride of place is given to a cross-sectional view of the male anatomy.
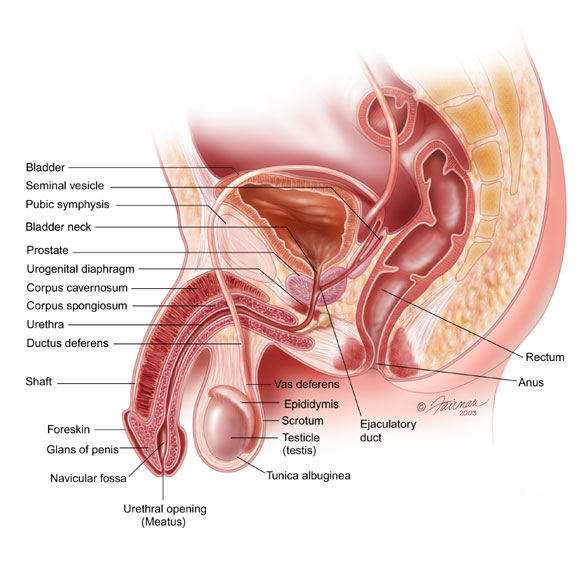
I’m not sure if this image is the one I get to stare at, but it’s a close match. I keep expecting some hints on the prime cuts and interesting ways to cook them.
I digress.
So, seated in the consultation room, I am informed that the Template Biopsy hasn’t disclosed any new frightening discoveries. In fact this latest biopsy pretty much supports the findings of the original TRUS (Trans Rectal Ultra Sound)(See Part 1 above). Basically my cancer is quite small, isn’t raging doesn’t on the face of it appear to be life threatening. In my words we are effectively back at square one. That is, the situation is the same as it was around 18 months before.
Relief
Obviously, I was quite relieved and commented to the consultant that I had fully expected to have to make a decision following the biopsy results. He was quite interested to know what my decision was going to be. I explained that I would probably have opted for the operation, prostate removal. My reasons being that I would be able to fall back on radiotherapy if the cancer reappeared. Once you have had radiotherapy surgery really isn’t an option.
Lecture
The consultants response to this was to give me a fairly forceful lecture on the possible side effects to the surgical option. Urine leakage and erectile dysfunction being the two headline leaders. He hammered home what a life changing thing incontinence can be and that I shouldn’t go into surgery lightly. For a surgeon he was doing a good job of selling radiotherapy to me. He then went on to explain to me what a difficult operation it is to remove the prostate.
Apparently my weight was a big consideration here and it was at this point he asked me to stand up so he could lift my shirt and demonstrate. He explained that for keyhole surgery, even though this isn’t abdominal surgery, the entry point is through the abdomen. Having entered the belly they then have to turn due south and head deep into the pelvic region. He pointed out that as I was a big lad, with a significant “food baby”, the journey through my entrails would be a long one. That he wouldn’t just have to negotiate his way past all the tubing but would probably have to burrow through extra fat. A new twist was that for the operation I would be tilted head down, meaning that all my fat encrusted viscera would slop up towards my lungs to press against my diaphragm. Wasn’t this a good thing I enquired, won’t this clear the way and make the operation easier. Nope, this migration makes life difficult for the anaesthetist. Yards of tubing heading north makes it difficult to keep the lungs full of oxygen. After this I wasn’t sure if he was bigging up his role or trying to dissuade me from having the surgery.
After all he is a surgeon, isn’t that his raison d’être. To be fair he did pretty much say that himself, that he just wanted me to be clear that surgery is not the easy option, nor is it without risks. I suppose I could have suggested that he had misjudged his audience since I was pretty well read up on the subject. I don’t let anyone go rummaging around my insides without finding out what they are supposed to be doing and what the pros and cons are.
Carry On Regardless
So, having come to an understanding I opted to carry on with the Active Surveillance with a view to probably having a scan and/or another biopsy. I must have given the impression that I wasn’t wholly convinced by his lecture and he was rather keen that I see one of his colleagues for an alternative view. This I agreed to do and we shook hands and parted company.
Approximately a month later I had an appointment with consultant number three. We discussed the biopsy results, the options open to me and the pitfalls of the various treatments. Once again it was agreed that I should carry on with the Active Surveillance. Part of the Active Surveillance regime is the taking of bloods on a regular basis, every 3 to 4 months, to monitor PSA levels.
PSA is not viewed as an accurate indicator of the presence of cancer but once diagnosis is confirmed the PSA can give an indication of change.
Changing Perspectives
And so it was I found myself once again at the QA, being given an opportunity to brush up my male anatomy and finally sitting in one of the consultation rooms. No consultant this time as I was seeing the Nurse Specialist. She talked me through my history and pointed out that my PSA levels had gone up. Previous readings had plateaued but the general trend was up. Her advice, based on 18 years of experience, and taking into account my age, she was of the opinion that it was time to take action. This was a contrast to the position taken by the consultants who were prepared to let me continue with the Active Surveillance. We kicked the subject around and it was agreed that I should go for a MRI scan and that I should then see the consultant to discuss the results.
MRI
If it’s good for nothing else, prostate cancer is introducing me to some new life experiences. TRUS, Template Biopsy and now an MRI. Everyone that I have spoken to, that has had an MRI, have said that they didn’t enjoy the experience. I wouldn’t say that I enjoyed it either but I didn’t actively dislike it either. I did, however, find it interesting. It’s noisy and a bit claustrophobic especially when you are my size. As your lower extremities disappear into the centre of the doughnut the hole begins to look a bit small. And when the table moves further in and your belly and chest further fill the available, visible, free space I suspect that the experience is similar to sausage meat being transported towards the sausage skin waiting on the tube at the outlet on the mincer. Another interesting thing I noticed was that as the MRI is clacking and clanking away the muscles in my left leg started to move in time with the noises. Not twitches as such, just a slight pull. Similarly, my wedding ring was also pulsing in time. These sensations varied with the tone of the MRI. Eventually it was all over and I left the QA to await the call to go and discuss the results.
Decision Time
Time moves on very quickly when you aren’t keeping an eye on it. Before I knew it I was back at the QA staring at that same wall with the same diagrams and posters. Still no recipes. And then into the consultation room.
Much to my surprise he told me that the results were really quite good. That is the MRI showed quite low levels of cancerous cells and that these cells do not appear to have moved onto other areas. All in all the MRI was pretty much repeating what the Template and TRUS biopsies had shown before. The only fly in the ointment was the steady upward trend of the PSA which didn’t seem to be echoing what the scan and biopsies were saying. Once upon a time doctors told you what was going to happen and then got on with it. In these PC times it’s all about patient choice. The trouble is the patient is necessary best qualified to make the decisions. Even if they have all the facts in front of the. And that’s the dilemma that i was confronted with.
I had the diagnostic results all laid out before me. I had all the options for treatment defined. I just had to make a decision.Anyone who knows me will know that I can’t make a decision when I’m in a restaurant with menu in hand. And then it doesn’t really have life changing implications if I make the wrong decision. Here there was no truly wrong decision to be made but the implications were momentous.
Decision Time
In the end I decided to go away and think on it. Subconsciously I probably knew what my decision was, but mentally I wasn’t ready to say it. I pondered for several weeks and then contacted the QA and told them to put me on the waiting list for surgery. The consultant had told me it would probably be a couple of months before I got a surgical appointment so I was looking at December / January.
Appointments & Disappointments
A couple of weeks ago, on a Tuesday, I got a call informing me that my appointment had been made. It was for the following Friday. Three days notice. Unfortunately I had other plans. The proposed day of the op we were due to go away over night and a week later we were heading up to Merseyside for a few days to spend time with family. Hotels had been booked and paid for and I wasn’t prepared to pass on those. The young lady tried to persuade me otherwise, telling me that “it’s really important that I had this operation”.
I wondered who she thought she was talking to. Wondered why she might think that I didn’t know the importance of the surgery. After all, I’m the one carrying the infected walnut around inside me. I’m the one going through the various biopsies, scans and blood tests. I’m the one who is being nagged by various family members to get on and have it done. She did, does, sound very young.
So, disappointed, she said she would call me again when they had another appointment for me. And that call came yesterday.
I have a busy week, next week. Monday I meet with the consultant. Wednesday I go for my pre-op meeting to see if i am fit to have the op. and Friday at 07:00 I have to present myself at Theatre reception.
I’ll let you know how I get on.
Part 5
Consultations
Monday I had a meet with my consultant. We reviewed my notes, discussed my latest blood test and the current PSA levels which are still high. This was not unexpected and I wanted to use this session to fill in answers to a number of questions buzzing around in my head .
How long would I be in hospital?
When could I get back to work?
When could I start driving again?
Some of the responses were a surprise.
My stay in hospital is likely to only be over night but I had previously been told 2 to 3 days. This is, of course, a good thing. The sooner I am back home the better.
Getting back to work is a much more difficult question to answer as there are many factors involved.
The first is the issue of continence or, to be more specific, incontinence. After the op I will be catheterised for a period of time, to allow the newly joined urethra to heal properly. Apparently, it can be quite uncomfortable when sitting, especially in a car. After the catheter is removed I will have to relearn bladder control and this can take quite some time. This is the main issue that made me so reluctant to have the op. Potentially pissing myself in a public place or in the workplace is a huge concept to deal with. Actually, in my mind, sitting in a restaurant with friends or family when my bladder decides to unleash a tidal wave of urine across the floor is probably my worst nightmare. Of course I am magnifying worst case scenarios, so anything less is actually a positive step.
Apparently fatigue is a common issue following the procedure. Not just tiredness but the inability to focus mentally.
The net of all this was that I would probably be away from the office for a few weeks.
My actual return to participating in work by working from home could be very much sooner.
It all depends on my body’s ability to recover. We are all different and our powers of recuperation so variable that it’s nigh on impossible to predict any outcome accurately.
At some point in the proceedings my consultant threw into the conversation that, not only would they be removing my Prostate, but they would likely harvest a few lymph nodes too. Apparently this is becoming a more common practice as analysis of the removed nodes can indicate if cancerous cells have started to migrate.
All good things come to an end and as my appointment was drawing to a close, the consultant suddenly left the room, returning with his hands full. Saying “These are for you ” he dropped a black bag into my hands. This was followed by a large tome similar to a filofax.
These, it transpired, were my initial starter pack of “tenna man” pads and helpful information regarding the after op time. In the filofax, more of the same, plus pages to record my diagnosis and treatment details.
Net result of this visit was confirmation of much that I already knew but also shows that there is no clear cut outcome for my forthcoming procedure.
Next step is the pre-op assessment….. Stay tuned 😉
Part 6
Pre Operation Assessment
Today found me back at the hospital again. This time for my pre-operation assessment.
The purpose of this assessment is to determine if I am fit enough to undergo a radical prostatectomy.
So, I was measured, weighed, prodded and squeezed. Gave blood, underwent an ECG and provided a pee sample. In addition I had to provide answers to 101 questions (or so it seems) on my past and current health. I had my clothes on and off more often than a professional stripper.
And with the completion of the assessment the countdown has started. Next stop, the operating theatre. Back at the Queen Alexandra Hospital, Friday morning @ 07:00
Part 7
December 5th, 2014 – Operation Day – An Early Start
05:15 and the alarm has awoken me from a crocodile infested sleep.
Time to get ready for my hospital trip.
Got to get spruced up for the nurses.
So have now been here for an hour. Waiting to see the surgeon and anaesthetist. And they asked me to come in early. Not happy.
Pretty much had to go through the pre-op assessment again as the notes taken on Wednesday were not in my file.
I just hope they remember what my operation is.
Part 8
December 5th, 2014 – A Stressful Day
My Prostate Operation Was Cancelled – After 3 + hours of waiting.
Well, it’s taken me a while to get my thoughts together after what turned out to be a really stressful morning. Truth be told, I had probably been stressing for quite a few days but had not realised……
As I said in my previous post, we had been requested to arrive thirty minutes earlier than the 07:00 originally planned. This was, supposedly, so that I could have my pre-operation meet with the surgeon and anaesthetist. So my wife and I dutifully presented ourselves at 06:30 in Theatre Admissions and were, almost immediately, shown through to a consultation room.
A nurse arrived, wrote out a luggage tag for my small holdall, and attached a fancier version to my wrist. So far all was moving along quite nicely. Next she started taking / checking my details and very soon I began to wonder what the point of the pre-operation assessment was since all the questions were repeats of Wednesday afternoons interrogation. My doubts further increased when she informed me that she didn’t have my blood details nor my ECG results both of which were part of the Wednesday session.
Already somewhat stressed, in anticipation of the forthcoming procedure, I was beginning to get a little terse. Not just that, but I was also beginning to wonder if they knew what I was in for. A thought that was reinforced a few minutes later when I was invited to get changed. Some of you will remember from my previous visit, for the template biopsy, that I had been given a gown which was way too small and couldn’t be secured. In an attempt to prevent the same indignity I asked for a larger gown. Yet again I was offered a small size. It was obvious that it wouldn’t even fit across my shoulders, let alone do up at the back. Almost grudgingly I was offered a “bariatric” gown. I muttered “whatever that is ” under my breath. Obviously not under enough, as I was informed “oh they are huge !!! “.
As she handed me my bell tent I was asked “what is it you are having done? ” I replied “my Prostate!! “. “Then you should take everything off!!” she informed me.
With that I was left to change. The gown had enough room in it to hold a small disco but at least I could fasten it up. And, best of all, my new dressing gown was of sufficient length to reach the lovely sage green pressure stockings I was sporting. This new vision of sartorial loveliness was finished off by my new suede moccasin style slippers. Now, properly attired, I returned to sit with my wife in the consultation room.
Meeting With The Anaesthetist
There then ensued a, seemingly, long wait. In truth it was probably only minutes but eventually the anaesthetist arrived and after he had confirmed my details, and repeated many of the questions from Wednesday afternoon, and from earlier this very morning, he ran through what the order of play would be.
For the first time the duration of the operation was mentioned. I had been under the impression that this was to be a two hour procedure. Nope, this was to be four to five hours in duration. Suddenly the first penny, of a whole bag full, dropped and the true magnitude of this operation began to sink in. Five hours!!! He also mentioned that it was possible that the robotic basis of the operation could switch to full open surgery should any problems arise. This had always lurked at the back of my mind and, to be honest, that is where I kept it filed. That is, until the session with the surgeon.
Fast forward a few minutes….
Meeting With The Consultant Surgeon
Mr. Wilkinson talked us through the operation and thoroughly explained risks. How little I knew. Over the last couple of years I have reviewed the implications of having this operation and thought that I was pretty well versed. Trouble is, I had been focusing on the post operative time frame. I had not paid too much attention to the detail of the surgery itself.
He, Mr Wilkinson, listed the various risks involved with a radical prostatectomy, starting with how difficult it was going to be to find the little sucker. Especially given the route taken during keyhole surgery, in through the abdomen then turn due south and head for the pelvic zone.
Add to that the fact that the robot has fixed length (but short) arms. I know some folks who are like that when it comes to buying their round in the pub. Next up was the proximity of the prostate to my bladder which introduces a risk of damage over and above the urinary incontinence which is to be expected. Moving swiftly on, next on the list is the proximity to the bowel.
New news here was that the prostate could be stuck to the bowel and that this could have been caused by, if not caused by then exacerbated by, the biopsies I had as part of the original diagnosis and active surveillance regime. At no time was it ever explained to me that the biopsies, TRUS or Template, could have negative impact on future surgery. Apparently during the prostate operation they mighty have to peel the bowel away from the prostate. The biopsies could contribute to any adhesion between the bowel wall and my prostate and the act of separation could cause damage that would have to be repaired. If such damage occurred it would require a colostomy to allow the repair to heal. Obviously, once the repair was healed there would have to be another operation to undo the colostomy. My four to six weeks recovery period suddenly looked to be extending with the possibility of the further surgery and recovery period.
Continuing on with the inherent risks of this surgery, let’s not forget that during the procedure I would be tilted head down by approximately 30 degrees. This would cause my innards to slop towards my head, thereby putting pressure on my heart and lungs. Apparently this is a negative thing.
The coup de grace was the underlying small print of robotic surgery, if they ran into any difficulties, i.e. the Da Vinci machines short arms couldn’t reach, they would revert to the good old fashioned procedure and open me up from stem to stern.
Bottom line for me was that, due to my 18.5 stone (259lb) weight, the risk factors were double the norm.
Anxiety
This operation, and the potential ramifications, was taking on mammoth proportions. And now, the anxiety I was already feeling, was ratcheting up to whole new levels. I really was beginning to feel that I was making a big mistake. But, despite my misgivings I still signed the consent forms.
You may well ask “Why?” Why proceed when I was obviously having doubts.
I can offer no sensible answer. Guilt, Fear, Not wanting to let anyone / everyone / myself down.
After Mr Wilkinson left, my wife said “I fully expected you to refuse to sign that “.
Her statement just added to my anxiety and it was at this point that the anaesthetist returned to ask if I would agree to an epidural. As there was the possibility of my robotic surgery converting to full open surgery he thought it might be a good idea to give me an epidural to help with the pain management.
It was then that I experienced what I can only describe as a “crisis “. It wasn’t that I was crying, there was no wailing and gnashing of teeth, just that my mind was in total turmoil. I was in a flat spin. I really don’t know if I was coherent but I do think I was borderline having a panic attack. I couldn’t answer him. I tried to explain that I was seriously thinking that I shouldn’t go ahead with the surgery. He sat there patiently until I regained my self control and eventually I informed him that he should go ahead with the epidural.
So I was still going ahead. I think that I probably convinced myself that it was normal to have doubts and that I was probably magnifying the issues out of all proportion.
Cancellation
At around 09:00, my wife, took herself off to work and I went to sit with the other surgical victims where I waited for nearly an hour. During this time I was brought a cup of tablets, my antibiotics, anti vomiting, anti anti everything etc etc. And a small cup of water to wash them all down. This was the only drink I had since 05:30. The nurse that delivered them said something that I didn’t quite catch but when I asked she apologised for the long wait and informed me that there was meeting underway to discuss if my operation was to proceed as there was an issue regarding availability of a bed for me after my operation.
Around 10:00 Mr Wilkinson arrived and took me off to a consultation room. He explained that my operation had been delayed due to the beds issue. That he and the other consultant, Mr Solomon, had decided at around 09:30 that the operation was a no go. At around 10:00 the management had given permission for the operation to proceed but by then this was considered to be way too late. The operating list for Friday was morning only, such a late start would mean changing members of the surgical team mid operation and a probable finish time around 17:00. Adding to the risks previously outlined and putting the surgical team under the clock, more so than they would normally be. All in all, not good for the patient, Me! And not good for them.
Relief
To say that I was relieved would be an understatement. I had a long chat with Mr Wilkinson about my earlier “crisis” and whether surgery was the right option for me. The net of this was that the reschedule of my operation would be deferred until after Christmas.
To be quite honest,my wife and I are taking this time to rethink if this is the right way to go. Right now it doesn’t seem that surgery is for me.
I think, fate was on my side, that this operation was never meant to be.
Part 9
See you all in six months !!!
For those of you who are following this saga you will remember that my last post was shortly after attending hospital for surgery. That the surgery was cancelled due to a lack of availability of beds.
I think the fates intervened and the cancellation of the operation was a blessing in disguise. There were just too many risks with the operation and the potential impact to my lifestyle for the following year (at least) were just too much to consider.
So, surgery, which was always my first choice, has now been kicked into touch, and became the option of last resort.
Since December 2014 I have had follow-up appointments with Mr Wilkinson, my consultant. We have discussed fully, my reasons for not going ahead with the surgical option. As a result I was referred to an oncologist, Mr Nagar who talked me through the alternative radiotherapy options.
- External Radiotherapy
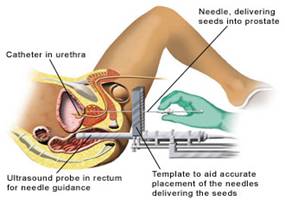
Given in the hospital radiotherapy department, as daily sessions from Monday–Friday, with a rest at the weekend. The course of treatment would last for just over 7 weeks. - Low-Dose Rate (LDR) Brachytherapy
This type of radiotherapy is sometimes called internal radiotherapy, implant therapy or seed implantation. This uses small, radioactive metal ‘seeds’ that are inserted into the tumour so that radiation is released slowly. The seeds are not removed but the radiation gradually fades away over about six months. There is no risk of it affecting other people.
So after a full and frank discussion with Mr Nagar I was left with a lot of thinking to do, along with more discussions with my wife. The net of this was that I decided that LDR Brachytherapy was the right treatment for me. The following images show the basics of the procedure.
And so it was back to Mr. Wilkinson who scheduled me for a Flow Rate Test. I mentioned that this was somewhat less than successful last time so he suggested that the fall back plan would be a visit to Urodynamics.
Flow Test
As preparation for the Flow Test I had to keep a diary, over three days, of how much liquid I took on board, the type of liquid (tea, beer, wine etc.) and how much pee I produced. On the day of the flow test I thought I would help things along by arriving at the hospital early and drinking lots of water. I spent nearly an hour walking the grounds sipping at my bottle of water. Twenty minutes before my appointment my bladder started to indicate that it would need emptying soon so I headed up to Urology. I let the receptionist know that I might have an urgent need to perform. I was directed to take a seat and to let her know when things became truly urgent. So I sat there and my bladder went to sleep.
At my allotted appointment time I was called through to another waiting area asked to sit, offered tea and told to shout when I was ready to do the test. My bladder snoozed on. It was perhaps another thirty minutes before my bladder woke up. So I looked for the nurse. No sign. Well she said to shout so I did. After all I didn’t want to waste this opportunity. Thankfully the nurse appeared and we dashed to the flow test equipment. Basically it looks something like this….

After successfully performing I was given a quick ultrasound check to see what was left in my bladder and there it was, job done. Although I had a second appointment set for a visit to Urodynamics it was deemed not to be necessary and was cancelled. Instead a new appointment with the consultant, Mr Hodgson, was set.
Time flew by and once again I presented myself for the scheduled appointment with Mr Hodgson. Sadly, not for the first time, there was a distinct lack of notes. At least the computer was working this time and he was able to access my notes that way. However, what was missing was the flow rate test results. Two sets of print outs were found from that date and I had to choose the chart from my test. Thankfully the graphs were very different and I could easily identify mine.
The results were deemed good and I was informed that I would need another rectal (digital) exam as well as having my prostate vital statistics taken.
So there I was again, trousers round my ankles, up on the couch, laid on my side with my knees under my chin. Different room but the scenery hadn’t changed just a blank wall painted in that neutral paint that all hospitals seem to choose.
First up was the rectal (digital) exam and for the first time since this whole process began I actually felt some discomfort, though not for very long. This was followed by an Ultrasound Scan during which measurements were taken of my prostate. These help to determine the shape and mass of the prostate and would be used during the Brachytherapy procedure.
Soon the scan was finished and I was back in the vertical plane. I almost had my trousers secured when I was informed that some of the data from the scan had not been saved. So it was trolleys round the ankles again, back on the couch and staring once again at the blandly painted wall. This time the scan image was saved and once fully dressed we were back to discussing the procedure and timing.
Apparently hospitals don’t keep a cupboard full of these things around and the seeds have to be procured. I wondered if they went to Suttons, Fothergills or perhaps our local garden center to obtain the seeds. I did not vocalise these thoughts. They implant 80 – 100 Iodine 125 seeds @ £30.00 each. That’s dearer than a packet of Impatiens seeds.
When my consultation was over I had to visit with the nurse for nasal & groin swabs. She was less than amused when I suggested that I had saved the NHS money by using one swab for both areas. Either she’d had a humour bypass or had heard it all before.
On 13th May I presented myself for my Pre-Op Assessment and was duly measured, weighed and gave up a blood sample.
Before I knew it a date had been set for the procedure, May 15th. This was sooner than anticipated and I will admit to going through a moment of panic.
On the day I presented myself at reception and was shown through to a consulting room. I was measured and weighed again, blood pressure taken and given some premeds, antibiotics etc.. I was visited by the anaesthetic and the consultant and signed the consent forms after having everything explained to me. Thankfully, this time, the wait was not very long between these consultations and being taken through to theatre.
Preparation for the procedure was a surreal experience, what with me being dressed in the wonderful hospital smock and stockings, also the jokey disposition of the theatre staff. We were actually having a good time and that was before I had any anaesthetic.
It was about this time that I started to misbehave. As usual they inserted a canula, except that they had two goes at that. Then they informed me that I was due to have an epidural, which had not been discussed previously. At the same time they administered something through the canula that they said would make me feel like I had consumed a couple of G & Ts. I remember feeling a little woozy and then nothing more until came to in the recovery area.
I was subsequently informed that the anaesthetists assistant tried on two occasions to set up the epidural. They are supposed to see spinal fluid come out of the needle and on each occasion I wouldn’t give any up. The anaesthetist then took over and tried herself, three more times, and still I wouldn’t give any fluid. At this point they decided that they would give up on the epidural and put me under with a general anaesthetic (GA). Once they had me under, and the procedure was underway, that’s when I really began to misbehave. I decided to vomit.
From what I have heard vomiting whilst under a GA is not good. This required the use of dyna-rod and a vacuum cleaner to clear out my tubes and the upper reaches of my lungs.
As a result of this the procedure took much longer than the estimated two hours which would be normal. A further consequence was that I had to stay in hospital overnight, when I had expected to go home, and I was wheeled up to a ward where I was connected to an oxygen supply with attached humidifier. This was so that they could monitor me and make sure that I hadn’t inhaled any of my stomach contents and didn’t suffer an infection.
So there I was stuck in hospital. Hungry, I hadn’t eaten for over twelve hours. Thirsty, no fluids other than a few sips of water prior to the procedure. Catheterised, for the procedure and for the duration of my observation. Sore throat due to the GA and subsequent rodding out and suction due to my vomiting session.
The nurses brought me a sandwich to alleviate the hunger. A cheese on wholemeal sandwich was the only choice and was so dry that it was very hard to swallow, especially kind to my sore throat …. NOT !!
This was only the beginning of the fun night. Did I mention that I was catheterised ? Through the night I was subjected to hourly obs. Just as I was drifting off to sleep along would come the nurse to take my temperature and my blood pressure. Then, just as I was drifting away again, she would come back and I would feel a pulling at my penis. This was specifically related to the brachytherapy and the catheter. She had to use a Geiger counter type device and scan the contents of bag attached to my catheter then along the length of the tube up to the old fella. Required to ensure that none of my seeds had escaped. Any found would need special handling for disposal. Seeds can escape from their implantation point and move around the body. Supposedly this is not harmful.
Saturday morning arrived and I felt a bit fresher after a strip wash and some breakfast. I was scheduled to go down for an X-ray but someone cancelled it which meant a new booking for later in the day. Hospitals are the most boring places to be when you are waiting to be released.
I was visited by the consultant who informed me that I would need to go for a scan on Monday. This was to ensure that the seeds were implanted in the right place and the right quantity. He also said I could have the catheter removed. Yippee !! His female assistant performed the removal saying “this might feel a little strange”. Decidedly unpleasant would have been my description. Mind you, after my first few pee’s following catheter removal I would have gladly had it back. The sensation is as close to burning as I can imagine and it seems like you can feel it all the way back to your bladder. Thankfully that sensation slowly faded away over the next couple of days.
The consultant also gave me a little blue card, which I have to carry for the next three years. This card informs people that I have “received a permanent radioactive iodine seed (Iodine – 125) implant to the prostate”. This is not because I glow in the dark, but the seeds will show up on various scanners and may even set off alarms at airports.
Back in the hospital, the consultant said he was happy for me to go home but that the final decision was down to the anaesthetist. And he wouldn’t give the go ahead until I had an X-ray.
Well it was nearly 16:00 when I was taken down for the X-ray and it was gone 17:00 before I was finally released. At this time I was given a box of Tamsulosin capsules.
Tamsulosin is used to relax the muscle around the Prostate which, not unexpected, can be a bit irritated following the implants. How would you feel after 80-100 foreign bodies were inserted about your person. Add to the facts that they are radioactive too. The irritation / inflammation can cause the Prostate to swell and constrict the urether making it difficult to pee.
So home I went. What a relief it was to get out of the hospital.
Part 10
So at the end of my last post I had just escaped from the QA following my Brachytherapy procedure. This was to be a temporary escape as I had to present myself back at the hospital for a CAT scan.
So the following Monday I dutifully presented myself for scrutiny. Unfortunately it was organised chaos due to a lack of availability of notes. This is not the first time that my notes have not been available although it is more usual for them to not be available for an appointment that has been set up for weeks.
I did press the radiographer as to why it was necessary for my notes to be available when they knew that the scan was to confirm placement of the radioactive seeds in my prostate. I said that I assumed they knew where the prostate was and therefore where to target the scan.
She, very patiently, explained to me that having a scan 3 days after brachytherapy was not normal procedure. The norm is to have an MRI after about a month, so they needed to know if there were any other issues that they needed to be aware of. They did their best to find my notes, even going up to the ward to search on the assumption that they, my notes, were “in transit” due to the weekend.
My consultant must have foreseen this as he had provided me with an extension number on which he could be contacted, even though he was in surgery. I passed this number over to the radiographer and after a short chat with my consultant we were good to go.
So after nearly two hours pfaffing around I had my ten minutes of scanning and we were out of the hospital. Of course there is then a period of trepidation, waiting to hear if I was going to have to go back in for more seeds. As time passed I relaxed, no news is good news after all.
A month after the procedure I had the MRI. This was a much quicker visit than my previous MRI. I guess because this time they were only interested in checking the prostate itself and the immediate surrounding area.
Once again, there is that trepidatious period of time where you wait for the bad news phone call. And, once again, as time passed I relaxed.
The next check point in all this was to be a visit to the consultant preceded by a visit to the vampire clinic.
Which brings us up to date.
Last week I gave the blood sample required to check my PSA levels and yesterday I visited my consultant. After all the pleasantries, how is your bladder, how are your bowels, etc. etc. we eventually got round to the important business i.e. talking about my PSA.
Brilliant news !!
Prior to the brachytherapy my PSA was up at just over 13. Now my PSA reads just over 1. Which, in the words of my consultant means that the seeds are doing their job. My next check point will be in six months when I will have another blood test and another consult.
My thanks to Clotho, Lachesis and Atropos, the three fates (Moirai) for watching over me. I think they were watching over me last December when my operation was cancelled due to a lack of hospital beds. When I think about all the possibilities I am so, so glad that I have taken this path.
See you all in six months !!!
Part 11
So said I, five years ago. A lot has happened in those five years although not a lot in the land of the prostate. Or perhaps I should say, not a lot, to my knowledge.
After our return from the latest Ozzie adventure, I was scheduled for a Urology Consult (telephone) 28th July, 2020. As is the norm, these are preceded by the taking of blood samples. As my GP had requested a blood sample to check my blood sugar levels, it seemed appropriate to combine them. So on Wednesday 22nd July, at eight in the morning, I presented myself at my local surgery and provided the necessary samples. I then sat back to await the consult scheduled for the following Tuesday. The next day, Thursday 23rd, I received a call from the GP surgery, could I come in and give another sample.
Apparently they wanted to rule out any potential issues with the analysis of the previous sample. As you can imagine my brain went into hyperdrive, what had the blood sample shown. I duly presented myself at the surgery and gave up some more of my blood. Although the person on the call didn’t know why I needed to give another sample, the nurse taking my blood was a little more forthcoming.
It appears the first sample showed my PSA level was up. This second sample was to determine if there had been a balls up in the lab or if something more sinister was happening.
Friday I received call from the surgery asking if I woud be prepared to have a telephone consult, with my GP Dr Mannings, on Tuesday evening. I pointed out that I also had a telephone consult with the Urologist on Tuesday morning. That’s great quipped the receptionist, you’ll be able to tell the doctor what the results are and what your urologists plans are.
With all this interest in my blood and doctors left, right and centre wanting to speak to me my curiosity was definitely peaked.
So Tuesday 28th duly arrives and I have my telephone consult with the Urologist, Mr Hodgson. Yes, he confirmed, my PSA has risen.
Apparently last June my PSA was 3.6 but these latest blood tests show my PSA at 7.9 and 8.9. A sure indicator that something is going on down in the nether regions although still lower than the 13.3 which was where I was at before having the Brachytherapy
Because of this my consultant wants me to have a series of scans. CT, MRI and full body bone scan. The call is ended with the promise that I will be contacted with appointment details.
Sure enough, later in the day I receive a call from the Scanning Dept., would I be available on the morning of Saturday 1st August, for a CT scan ? Yes of course, and so I am duly booked in for 09:00.
Later the same day I have my consult with my GP. He already knew about the consultants plans but is like a child being handed a bag of sweets, so excited, when I tell him that already have the first of my scans booked.
The NHS is actually working very swiftly and efficiently. Obviously I have Covid-19 to thank for this, the hospitals are operating in a very stripped back mode. All to my advantage.
Over the next few days I receive calls and set up the remaining appointments. Monday 3rd August @ 19:00 for the MRI and Tuesday 11th August for Full Body Bone Scan. The bone scan is in two parts. I have to turn to at 11:15 for a radioactive injection. Go away for a while, then return at 14:30 for the actual scan. Apparently, after the injection, due to its radioactive nature, I have to steer clear of any pregnant women and young children Same advice I was given after I had my Brachytherapy.
I duly attended the three scans. One thing I noted is that I am able to lay completely still during these scanning sessions. They each have taken anything between twenty minutes and forty five minute. At home I find it just about impossible to keep my legs still, whether I am sitting watching TV or laid in bed. Maybe I need to get a huge doughnut installed at home.
For each of the scans I also had an injection. The one administered during the CT, I was warned, would trigger a warm sensation in my nether regions. Something akin to wetting oneself. Not something you want to consider when typically any sensation in the bladder region typically turns into a pee panic. As it happens, the sensation I felt was around the neck and up around my ear. Something like I used to feel when my Mum had caught me out in a lie. For the MRI I was given an injection of Buscopan. When I mentioned that my wife takes Buscopan for her IBS te doctor said it’s the same stuff but won’t hang around as long but that it might affect my eye sight i.e. blur my vision. He assured me it would have cleared my system before I got back to my car for the drive home. As for the bone scan and the radioactive injection I was informed that, other than having to stay away from pregnant ladies and young children, there were no side effects, that I wouldn’t be aware of it in my bod.
All that remained was for me to await the results. I assumed that I would receive a phone call from my consultant, Mr Hodgson.
I did receive a phone call, but not from Mr Hodgson. It was from a yong lady, I assume from the Urology Department reception.
She informed me that she was calling to book me in for a Pre-op Assessment !!!
My heart dropped, my stomach did a flip.
“Pre-op ?” I said, “pre-op for what ?”
“Well, you came into Urology yesterday” says the young lady.
“Nope” says I, “I didn’t, I haven’t had any contact with Urology since the 28th July”.
“Oh !” she says “And you haven’t seen the letter ?”
Again “Nope” says I, “In fact I would have expected a phone call from Mr Hodgson, not a bloody letter”.
She is really apologetic and puts me on hold briefly. When she comes back on line she asks me if I want to wait for the letter, or she could read it out to me. I take the latter option. So, she reads the letter to me. My heart and stomach resume a more calm state.
None of the three scans suggest any spread of the disease.
Needless to say, this news was not what I was expecting. Nevertheless, it was encouraging. The letter, from Mr Hodgson, set out the next steps to be taken to determine if in fact my cancer has recurred.
Those steps are ..
- PET CT
- Template Biopsy (to be carried ot under GA and the reason for the Pre-Op)
The PET CT has been scheduled for Tuesday 25th August @ 15:00 and I have had the Pre-Op. This was in two parts. Part 1 was on Tuesday 18th, a telephone assessment which was then followed up with a hospital visit on Thursday 20th, where they carried out an ECG, swabs for MRSA and took a urine sample.
So there we are, all up to speed. I’ll post my next episode after the PET CT and when I know the date for the biopsy ……
Part 12
Well here we are again. After another long hiatus, I thought it was time to update you all. The lack of posts on this subject is purely down to, in part, happenstance and in part, inertia on my part. So, for that, I apologise.
So, my last post was back in 2020, following a five year hiatus. Only 28 months this time, I must be improving.
My previous post ended with me waiting for various scans, which were duly carried out, as follows:
- 1st August 202 – CT Scan
- 3rd August 2020 – MRI Scan
- 11th August 2020 – Bone Scan
- 25th August 2020 – PET CT Scan
Much as I like playing with all the NHS toys, I could do without the palaver of driving to the hospital, searching for a parking space, then waiting for my turn in the scanning department. Don’t get me wrong, I am very grateful for the attention that I am getting. Anyway, the net result of all these scans was, overall, a positive one. The scans indicating that there was no sign of the cancer around the prostate itself, and, apparently, no sign of metastasis. Prostate cancer apparently tends to migrate to the bones, or so I believed. So also getting the all clear from the bone scan was a positive thing.
Or, maybe the prostate cancer was hiding ?
Although there was no sign of the cancer around the prostate or in my bones, they did discover something in my lung !!! I became aware, very recently, that Prostate Cancer can metastasise to the lungs. So my case became the subject of one of the hospitals multi-disciplinary meetings.
Apparently there was much chin and arse scratching, bone tossing and probably some discussion about how Pompey were doing in the football league. The net is that my urologist talked to the chest doctors. They, the chest doctors, suggested that, whatever it was, was in a difficult to reach place. They further suggested that “we” should wait for 6 months and then have another scan. Then decide what steps to take.
My man, the urologist, didn’t think that was such a good idea. He felt, if this was the prostate cancer, it would be better to be proactive and treat it accordingly. Consequently he decided to start me on a course of Prostap injections.
And so it was that, on the 14th October, 2020, I started my course of Prostap. One injection every 4 weeks. This continued until November of 2021.
During this time, continuing blood tests and a scan showed the “thing” in my chest had shrunk and my PSA levels were dropping. In the words of my urologist, the “thing” had self diagnosed itself to be Prostate cancer. So we continued on with the Prostap jabs until, following a conflab with my urologist, we decided that I should take a break.
Apparently Prostap, along with most medications, comes with its own baggage. One potential side effect is the impact to ones bones, increasing the possibility of osteoporosis. With everything else that’s going on I certainly didn’t need that in my life.
I continued having blood tests to monitor my PSA and each of those was followed up with a telephone consult with my urologist. Always a very pleasant few minutes chatting followed by wishing each other well until the next call.
Latterly the calls included a concern about the fact that my PSA levels were bouncing around up to a new high of 3.2. Thats up from the zero point something I was at once the initial Prostap course was well underway.
At the end of August 2022, during a telephone consult with my urologist, it was decided that I should restart the Prostap injections. I had the first of the new course at the end of September. This time round the jabs are on a 3 month cycle and my next one is scheduled for March.
Following the last blood test, the Prostap, after only 3 months, appears to be working its magic. My current PSA level is 0.4 Great news by any measure..
From initial diagnosis, Brachytherapy in 2015 and thru to Prostap it has been an interesting experience. If, in the future, I have anything significant to report I’ll post again.
Before I go, I would like to thank all of the NHS staff who have handled my various visits to and stays in the Queen Alexandra Hospital, Portsmouth. You have, thus far, been amazing.
The journey, certainly isn’t over, but for now that is it.


Any news regarding the results yet Bob? Thinking of you…..
Hi, I had a full prostate op 5 years ago at 46! Well done for sharing your experiences. All the best…Graham
Hi Graham, Thanks for visiting. Hope all is still well with you following the op. Cheers Bob